PC – Platelet Count: Methods, Merits & Demerits
About Platelet:
- Platelets, also known as thrombocytes, are small, anucleated blood cells essential for blood clotting and maintaining vascular integrity.
- A platelet count is a part of the Complete Blood Count (CBC) and is vital in diagnosing bleeding disorders, thrombocytopenia, thrombocytosis, and monitoring therapies like chemotherapy or anticoagulant use.
Normal Platelet Count
-
Adults: 1.5 – 4.5 lakh/cu mm (150,000 – 450,000/µL)
-
Newborns: 1.0 – 4.5 lakh/cu mm
-
Critical Values:
-
Below 20,000/µL: Risk of spontaneous bleeding
-
Above 10 lakh/µL: Risk of thrombosis
-
Functions of Platelets
-
Initiate clot formation (hemostasis)
-
Maintain endothelial integrity
-
Involved in inflammation and wound healing
Methods of Platelet Count Determination
- Manual Method (Rees-Ecker Method / Improved Neubauer Chamber Method.
- Automated Platelet Count (Hematology Analyzer)
1. Manual Method (Rees-Ecker Method or Improved Neubauer Chamber Method)
Principle:
- A diluting fluid is used to lyse RBCs and stain platelets.
- The diluted blood is then charged on a Neubauer counting chamber, and platelets are counted under a microscope.
Rees-Ecker Method (Manual Count)
Reagents:
-
Rees-Ecker diluting fluid:
-
Sodium citrate – prevents clotting
-
Brilliant cresyl blue – stains platelets
-
Formalin – fixes platelets
-
Distilled water – diluent
-
Procedure:
-
Mix fresh anticoagulated blood (EDTA) with diluting fluid in a 1:200 dilution.
-
Fill the Improved Neubauer hemocytometer with the diluted sample.
-
Allow platelets to settle for 10–15 minutes.
-
Count platelets in the entire central large square (25 small squares).
-
Multiply the number of platelets by the dilution factor to get platelet count per µL.
Merits:
-
Inexpensive
-
Does not require automated analyzers
Demerits:
-
Time-consuming
-
Platelets may clump or be confused with debris
-
Needs good microscopy skill
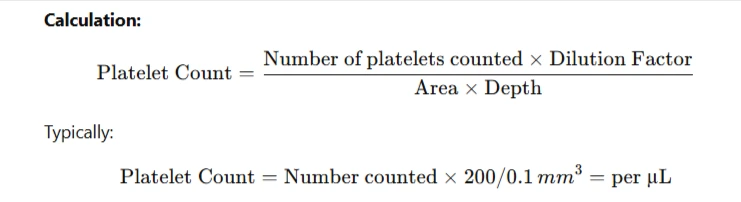
Calculation:
2. Automated Platelet Count (Hematology Analyzer)
Principle:
- Uses electrical impedance or optical flow cytometry.
- Platelets are counted based on size and internal complexity.
Procedure:
Whole blood is aspirated by the analyzer.
Platelets are distinguished from RBCs and WBCs by size and counted electronically.
Results displayed along with other CBC parameters.
Merits:
- Accurate, fast, and reproducible
- No observer bias
- Can also provide Platelet Distribution Width (PDW) and Mean Platelet Volume (MPV)
Demerits:
- Expensive equipment
- May misclassify clumped platelets or large platelets
- Requires maintenance and electricity
3. Peripheral Blood Smear (Cross-check Method)
Principle:
Estimate platelet count by comparing them with RBCs under oil immersion in a stained smear (Leishman/Wright).
Procedure:
Prepare and stain a thin blood smear.
Under oil immersion (100x), count platelets in 10 fields.
Average number per field × 15,000 = Approximate count per µL.
Merits:
- Simple
- Helps detect clumping or morphological abnormalities
Demerits:
- Rough estimation only.
- Subjective and not suitable for precise counting
Causes of Abnormal Platelet Count:
| Condition | Count | Examples |
|---|---|---|
| Thrombocytopenia | Low (<150,000) | Dengue, leukemia, bone marrow failure, ITP |
| Thrombocytosis | High (>450,000) | Infections, iron deficiency, myeloproliferative disorders |
Sources of Error
- Clotted sample
- Platelet clumping (EDTA-induced)
- Misidentification of debris or cells
- Inadequate mixing of blood before sampling
Precautions
- Use fresh EDTA blood (<2 hours old)
- Mix well before testing
- Avoid hemolysis
- Clean counting chamber and cover slip